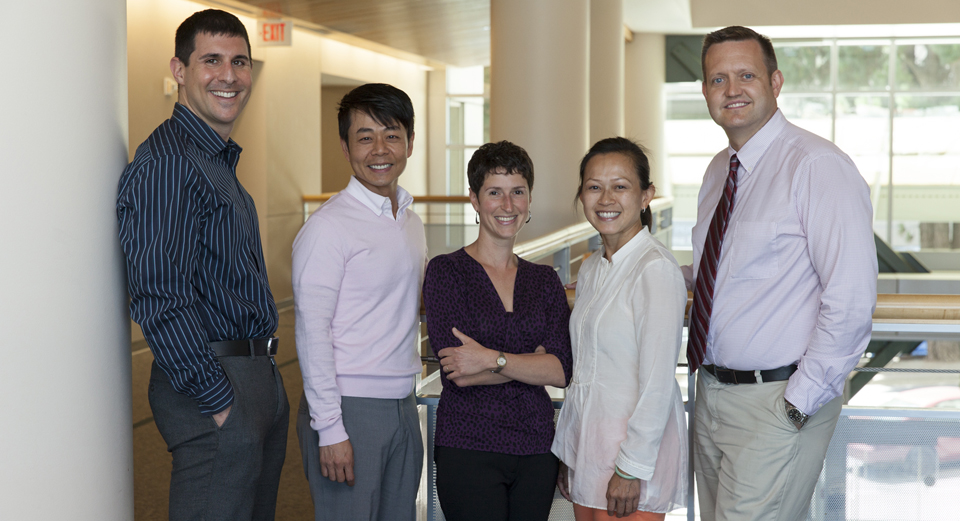
Kaiser Permanente researchers did a large, ‘real-world’ study of a pill used to prevent HIV infection, and found no new infections. The study’s team includes (left to right): Jonathan Volk, MD, MPH; Tony Phengrasamy, PharmD; Julia Marcus, PhD, MPH; Dong-Phuong Nguyen, PharmD; and C. Bradley Hare, MD.
In one of the first and largest published evaluations of the use of a single pill to prevent HIV infection in a clinical practice setting, researchers at Kaiser Permanente found no new HIV infections among patients using preexposure prophylaxis (PrEP) during more than 2.5 years of observation. The study was published in Clinical Infectious Diseases.
“Our study is the first to extend the understanding of the use of PrEP in the real world and suggests that the treatment may prevent new HIV infections even in a high-risk setting,” reported lead author Jonathan Volk, MD, MPH, physician and epidemiologist at Kaiser Permanente San Francisco. “Until now, evidence supporting the efficacy of PrEP to prevent HIV infection had come from clinical trials and demonstration projects.”
In 2012, the U.S. Food and Drug Administration approved a fixed-dose treatment of the antiviral drugs emtricitabine and tenofovir for daily use in combination with safer sex practices as a way of preventing HIV infection in people who do not have HIV but are at high risk of getting it. When someone is exposed to HIV through sex or injection drug use, these medications, in a single pill commercially known as Truvada, can keep an infection from becoming established.
Over the 32-month observation period at the Kaiser Permanente Medical Center in San Francisco, there were 1,045 referrals for PrEP and 657 people who began the PrEP regimen. The average length of use during the study period was 7.2 months, resulting in 388 person-years of observation of PrEP use. The average age of PrEP users was 37, and 99 percent were men who have sex with men (MSM). Compared with people who decided not to start PrEP, users were more likely to report multiple sex partners.
Of 143 patients who were asked about behavior change after six months of PrEP use, the number of sexual partners was unchanged in 74 percent, decreased in 15 percent, and increased in 11 percent. Condom use was unchanged in 56 percent, decreased in 41 percent, and increased in 3 percent.
At six months after initiation, 30 percent of PrEP users had been diagnosed with at least one sexually transmitted infection (STI). At 12 months, 50 percent of PrEP users had been diagnosed with any STI.
“Without a control group, we don’t know if these STI rates were higher than what we would have seen without PrEP,” said co-author Julia Marcus, PhD, MPH, postdoctoral fellow at the Kaiser Permanente Division of Research. “Ongoing screening and treatment for STIs, including hepatitis C, are essential components of a PrEP program.”
According to senior author Bradley Hare, MD, director of HIV Care and Prevention at Kaiser Permanente San Francisco, people on a PrEP regimen should also be tested frequently for HIV infection, as well as for side effects of Truvada, including changes in kidney function.
While researchers observed that demand for PrEP is growing among MSM, they also underscored the need for outreach to others at risk for HIV, including transgender women, heterosexual men and women, and people using injection drugs.




This Post Has 2 Comments
Great article. Thanks for sharing the information.
View your list of medications from your Kaiser Permanente medical record and set reminders to help you remember how much medication to take and when to take it.